Low Back Pain
Overview: The lumbar spine supports most of the body’s weight, making it prone to pain. Low back pain can vary from dull aches to sharp, shooting sensations that affect mobility.
Symptoms: Common symptoms include pain in the lower back, difficulty standing or moving, and sometimes numbness or tingling in the legs. In severe cases, muscle weakness or loss of bladder control may occur.
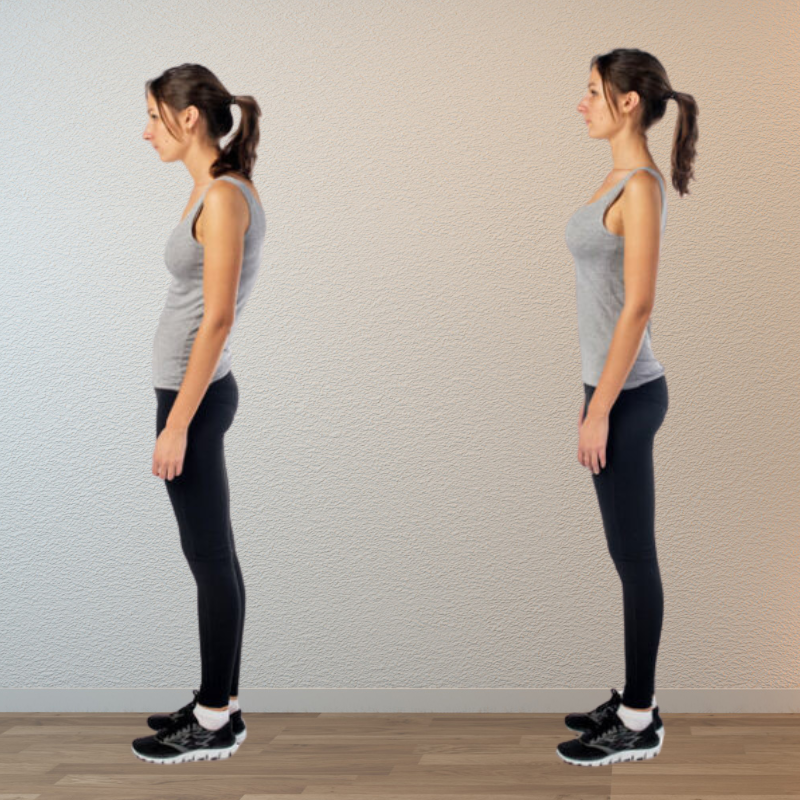
Causes: Low back pain can result from muscle strain, poor posture, or injury. Conditions like herniated discs, arthritis, or spinal stenosis can also contribute to pain.
Diagnosis: A physical examination and imaging tests such as X-rays or MRIs help identify the exact cause of pain and determine the best treatment plan.
Treatment: Treatment includes physiotherapy, pain medications, and lifestyle changes. For severe cases, surgery may be considered, though it's typically a last resort.
Neck Pain
Overview: Neck pain occurs due to issues in the bones, muscles, nerves, and joints, often leading to discomfort in the head, shoulders, and arms.
Symptoms: Pain, stiffness, muscle tightness, headaches, and numbness or tingling sensations.
Causes: Poor posture, aging (arthritis), herniated discs, injuries (e.g., accidents), or underlying diseases like autoimmune disorders.
Diagnosis: Includes physical exams, X-rays, CT scans, and MRIs to detect the extent of damage and underlying causes.
Treatment: Can involve medications, physiotherapy, posture correction, cold/heat therapy, and in rare cases, surgery for nerve or spinal compression.
Sciatica
Overview: Sciatica is nerve pain caused by injury or irritation to the sciatic nerve, which originates in the gluteal area. It usually describes pain starting in the lower back and radiating down the leg. The sciatic nerve, the longest in the body, runs from the hips down each leg, branching into nerves reaching the foot and toes.
Symptoms of Sciatica: Sciatica typically causes pain radiating from the lower spine to the buttock and down the leg. Symptoms may include muscle weakness, numbness, or tingling in the leg, ranging from mild discomfort to sharp, electric-shock-like pain, often worsening with movement. Severe cases may involve loss of movement or bladder control.
Causes of Sciatica: Sciatica can be caused by various conditions:
- Herniated Disc: The most common cause, where intervertebral discs bulge or rupture, compressing the sciatic nerve.
- Spinal Stenosis: Age-related narrowing of nerve passageways pinches the sciatic nerve roots.
- Spondylolisthesis: Misaligned vertebrae narrow nerve openings, pinching the sciatic nerve.
- Bony Spurs: Inflammation over time forms protrusions that can compress nerves in the lower back.
- Trauma: Spine injuries may damage or pinch the sciatic nerve.
- Cauda Equina Syndrome: A rare, serious condition affecting the spinal cord’s nerve bundle, causing leg pain and loss of bladder control.
Diagnosis: Sciatica diagnosis involves medical history, physical examination, and possibly imaging, such as X-rays, CT scans, or MRIs, to detect degenerative changes or nerve impingement.
Treatment: Treatment focuses on reducing pain and improving mobility. Many cases improve with self-care, such as hot/cold compresses, OTC pain relief, and stretches. Further treatments may include physiotherapy, steroids, or postural adjustments. Severe cases may require surgery, often minimally invasive. Get Treatment
Spinal Stenosis
Overview: Radiculopathy occurs when nerves are pinched or damaged as they exit the spine. It can cause pain, numbness, or weakness depending on which nerve is affected.
Symptoms: Pain, weakness, or numbness may radiate to the neck, back, arms, or legs. In severe cases, bowel or bladder control may be lost.
Causes: Radiculopathy can be caused by:
- Herniated Disc: Disc damage pressing on nerve roots.
- Bone Spurs: Extra bone growth compressing nerves.
- Spinal Stenosis: Narrowing of spaces around the spinal cord.
Diagnosis: Diagnosis involves a physical exam, imaging tests, and nerve function tests like MRI or CT scans.
Treatment: Non-surgical treatments like pain medications, physical therapy, and cold/hot compresses can help. In severe cases, surgery may be needed to relieve pressure on the nerve. Get Treatment
Foraminal Stenosis
Overview: Foraminal stenosis occurs when the foramen, the space through which nerves exit the spine, narrows and pinches the nerves. This condition is common, especially in older adults.
Symptoms: Symptoms vary based on the location of nerve compression. Cervical stenosis causes neck and arm pain, while lumbar stenosis leads to pain, tingling, or weakness in the legs. Sciatica is often associated with lumbar stenosis.
Causes: Foraminal stenosis can result from:
- Herniated Discs: Damaged discs pressing on nerve roots.
- Bone Spurs: Growths that narrow the foramen.
- Arthritis: Degeneration of the spine and its structures.
Diagnosis: A physical exam and diagnostic imaging like X-rays, MRIs, or CT scans are used for diagnosis. Nerve function may also be evaluated through tests like electromyography (EMG).
Treatment: Most cases are treated with pain relief, physical therapy, and activity modification. Steroid injections may help reduce inflammation. In severe cases, surgery such as foraminotomy may be necessary to relieve pressure on the nerve. Get Treatment
Lateral Recess Stenosis
Overview: Lateral recess stenosis occurs when the lateral recess, a space near the nerve roots, narrows and compresses nerves. This form of spinal stenosis may coexist with other spinal issues.
Symptoms: Symptoms are related to nerve compression and can include pain, weakness, and tingling in the affected area. Neck stenosis may cause sharp pain that radiates to the shoulders and arms, while lumbar stenosis affects the legs and feet, often resulting in sciatica.
Causes: Common causes of lateral recess stenosis include:
- Herniated Discs: Damaged discs pressing on nerve roots.
- Bone Spurs: Growths that narrow the lateral recess.
- Arthritis: Degeneration of spinal structures narrowing the space.
Diagnosis: Diagnosis includes a physical examination, medical history, and imaging studies such as X-rays, MRIs, or CT scans to evaluate the degree of stenosis.
Treatment: Treatment starts with conservative measures like pain relief, physical therapy, and rest. Surgery, including procedures like laminectomy or foraminotomy, may be necessary for severe cases. Get Treatment
Vertebral Compression Fractures
Overview: Vertebral compression fractures (VCFs) occur when the vertebral body collapses, most commonly in the thoracic and lumbar spine. These fractures are often associated with weakened bones, such as those caused by osteoporosis.
Causes: Common causes include:
- Osteoporosis: Weak and brittle bones make them prone to fractures.
- Trauma: Falls, lifting heavy objects, or car accidents can cause fractures.
- Spinal Infections: Can weaken vertebral bones.
- Spinal Tumors: May lead to fractures.
Symptoms: Common symptoms of VCFs include:
- Back pain
- Numbness and weakness in arms and legs (in cases with nerve impingement)
- Increasing pain while walking or standing
- Loss of height and spinal deformity
Diagnosis: Diagnosis involves a medical history review, physical examination, and diagnostic imaging. X-rays can show decreased vertebral height and fractures, while MRI or CT scans may be used if symptoms worsen despite treatment.
Treatment: Treatment options include:
- Conservative Treatments: Physical therapy, pain relief through medications like NSAIDs, and back strengthening exercises.
- Surgical Options: Vertebroplasty (injecting bone cement) and Kyphoplasty (using a balloon to inject cement) are considered for patients who don't respond to conservative treatment.
Spinal Tumours
Overview: Spinal tumours are abnormal growths within the spine, classified into primary and secondary (metastatic).
Types: Intramedullary, Extradural, and Intradural-Extramedullary.
Causes: Risk factors include genetic conditions, immune deficiencies, and exposure to carcinogens.
Symptoms: Back pain, radiating pain, weakness, and bladder/bowel issues.
Diagnosis: Diagnosed with physical exams, X-rays, CT scans, and MRIs.
Treatment: Includes surgery, chemotherapy, and radiotherapy depending on tumour type and severity.
Spinal Trauma Surgery
Overview: Spinal trauma can damage the spinal cord and vertebrae, leading to instability and fractures. Surgery is required to decompress the spinal cord and stabilize the spine.
Indications: Surgery may be needed for unstable fractures, flexion injuries, sacral fractures, or spinal compression.
Procedure: Minimally invasive surgery can include decompression to relieve pressure or stabilization with implants. Fusion may be used to promote healing.
Post-op Care: Expect soreness, but pain can be managed with medication. X-rays may be used to track progress. A calcium-rich diet is recommended for bone healing.
Recovery: Recovery can take up to one to two years, with the fastest improvement in the first six months.
Paediatric spine diseases
Overview: Paediatric spine diseases include deformities like spina bifida and tethered cord syndrome, occurring during development or birth.
Common Types: These include spina bifida (meningocele, myelomeningocele) and tethered cord syndrome.
Causes: Genetic factors, folic acid deficiency, and environmental factors such as viruses, diabetes, and obesity contribute.
Diagnosis: Diagnosis is through prenatal screening (ultrasound, amniocentesis), imaging (MRI, CT), and blood tests.
Treatment: Treatment may involve surgery, mobility aids, and addressing related conditions like hydrocephalus.
Cranio-vertebral Junction Anomalies
Overview: CVJ anomalies involve the base of the skull and upper cervical spine, often congenital or secondary to diseases.
Causes: These include skeletal abnormalities, congenital disorders (e.g., Achondroplasia), infections, tumors, and trauma.
Symptoms: Symptoms include neck pain, headaches, and reduced movement. Severe cases may cause spinal cord compression or brainstem dysfunction.
Diagnosis: Diagnosis is made through medical history, physical exams, and imaging (X-rays, CT scans, MRIs).
Treatment: Treatment typically involves surgical intervention, including reduction, decompression, and fixation.
Kyphoscoliosis
Overview: Kyphoscoliosis is an abnormal curvature of the spine in both the sagittal and coronal planes, often with rotation.
Causes: Causes include idiopathic origins, congenital malformations, degenerative changes, fractures, and neuromuscular conditions.
Symptoms: Symptoms can include back pain, stiffness, uneven shoulders, and hunched back. Severe cases may lead to respiratory or neurological complications.
Diagnosis: Diagnosed through medical history, physical exams, and imaging (X-rays, MRIs).
Treatment: Non-surgical options include physical therapy, pain management, and observation. Severe cases may require surgery such as spinal fusion.
Bone Spurs
Overview: Bone spurs (osteophytes) are bony growths that form in joints, often as a result of wear and tear. They are commonly found in the spine, neck, and joints like knees and hips.
Symptoms: Symptoms may include neck or back pain, numbness, tingling, and weakness in the limbs. These occur when spurs compress nearby nerves.
Causes: Common causes of bone spurs include:
- Osteoarthritis: Cartilage breakdown leading to spurs.
- Spinal Injuries: Damage to the spine triggering bone growth.
- Degenerative Disc Disease: Disc wear leading to spur formation.
Diagnosis: Bone spurs are diagnosed through a physical exam and imaging tests such as X-rays, MRIs, or CT scans to evaluate nerve involvement.
Treatment: Most cases are treated with physical therapy, medications, and injections. In severe cases, surgical procedures like laminectomy or foraminotomy may be required. Get Treatment
Discitis
Overview: Discitis is an infection of the spinal discs causing back pain and discomfort. It can result from direct infection or spread from other parts of the body.
Symptoms: Common symptoms include severe back pain, stiffness, fever, and localized pain in the infected disc area. Pain worsens with movement.
Causes: Discitis can be caused by bacterial, viral, or fungal infections, often due to previous spinal procedures or infections spreading from other body parts.
Diagnosis: Diagnosis involves physical exams, blood tests for infection, and MRI scans to confirm infection.
Treatment: Treatment typically includes antibiotics, pain relief medications, bed rest, and sometimes surgery for severe cases.
Cervical Spondylosis
Overview: Cervical spondylosis is the age-related wear and tear of spinal discs and joints in the neck. It affects over 85% of people over 60 years.
Symptoms: Common symptoms include neck pain, stiffness, headaches, tingling, and muscle weakness. Pain often worsens with neck movement.
Causes: Causes include loss of disc fluid, bone overgrowth, disc herniation, and ligament stiffness. Risk factors include age, neck injuries, poor posture, and obesity.
Diagnosis: Diagnosed through medical history, physical exams, and diagnostic imaging such as X-rays, CT scans, and MRIs.
Treatment: Treatment includes physical therapy, pain medications, cervical collars, and in severe cases, surgery such as discectomy or laminectomy.
Lumbar Spondylosis
Overview: Lumbar spondylosis is age-related wear and tear in the lower back’s spinal discs and vertebrae, leading to pain and discomfort.
Symptoms: Symptoms include lower back pain, stiffness, radiating pain to legs, tingling, and muscle weakness.
Causes: Causes include aging, lower back injuries, prolonged sitting, obesity, and strenuous spinal movements.
Diagnosis: Diagnosed through physical exams, neurological evaluations, CT scans, and MRIs to detect bone growths and soft tissue issues.
Treatment: Treatment options include physical therapy, medications, injections, and in severe cases, surgery like spinal fusion or decompression.
Degenerative Disc Disease
Overview: Degenerative disc disease involves wear and tear of spinal discs, common with aging. It affects spinal mobility and can lead to pain, especially in the back and neck.
Symptoms: Symptoms include sharp back or neck pain, tingling, numbness, and radiating pain to limbs. Pain often worsens with certain movements or postures.
Causes: Key causes are age-related disc wear, injuries, and loss of disc fluid. Risk factors include poor posture, obesity, and smoking.
Diagnosis: Diagnosis is based on medical history, physical exams, and imaging tests like X-rays, CT scans, and MRIs.
Treatment: Treatment includes pain management, physical therapy, lifestyle changes, and surgery for severe cases, such as spinal fusion or disc replacement.
Facet Joint Pain
Overview: Facet joint pain is caused by wear and tear of the spinal joints, often seen in people aged 40-70. It can cause significant back and neck pain.
Symptoms: Symptoms include dull aches, pain during movement like bending or twisting, and radiating pain, often in the neck, mid-back, or lower back.
Causes: Causes include age-related cartilage wear, injury, poor posture, and obesity. The pain can worsen with repetitive movements or pressure on the spine.
Diagnosis: Diagnosed via physical exams and imaging tests like X-rays, CT scans, and MRIs. These help evaluate bone and tissue damage.
Treatment: Treatment involves pain medications, physical therapy, joint injections, and lifestyle changes. Surgery may be necessary for chronic pain or nerve compression.
Disc Bulge
Overview: A disc bulge occurs when the outer layer of an intervertebral disc extends beyond the vertebrae, often due to aging or trauma. It can lead to nerve compression and other spinal issues.
Symptoms: Symptoms may include pain, tingling, numbness, or weakness, depending on the affected disc. Severe cases may result in conditions like sciatica.
Causes: Bulging can result from disc degeneration, improper lifting, repetitive strain, or trauma. Risk factors include obesity, genetics, and smoking.
Diagnosis: Diagnosed through a physical examination and imaging studies such as X-rays, CT scans, or MRIs to assess the extent of degeneration.
Treatment: Treatments may include pain management, physiotherapy, and in severe cases, minimally invasive surgery like endoscopic surgery to remove the protruding disc.
Disc Tear
Overview: A disc tear involves a thinning or rupture of the intervertebral disc, categorized into annular tear and disc rupture. It can cause nerve irritation and pain.
Symptoms: Symptoms vary by location, but may include pain, numbness, or weakness in the arms or legs, with sharp or burning sensations.
Causes: Common causes include aging, improper lifting, or trauma. Risk factors include excess weight, strenuous work, genetics, and smoking.
Diagnosis: Diagnosed through medical history, physical exams, and imaging tests like X-rays, CT scans, or MRIs.
Treatment: Non-surgical treatments like pain medication and physical therapy are common. In severe cases, surgery such as discectomy or endoscopic procedures may be needed.
Intervertebral Disc Health
Overview: Intervertebral discs are shock absorbers between vertebrae, with an outer fibrous ring and inner gel-like nucleus. These discs help with flexibility, movement, and pressure distribution.
Common Issues: With age, discs can degenerate, causing conditions like bulging, herniation, and annular tears. These changes may result in pain and reduced flexibility.
Causes: Disc degeneration can be worsened by age, poor posture, heavy lifting, and lack of exercise, leading to pain and potential nerve compression.
Symptoms: Symptoms include back pain, numbness, and weakness, especially during movement or pressure on nerves.
Treatment: Treatment options include physical therapy, pain medications, and in severe cases, surgery like discectomy or micro-discectomy.
Ravi Philips
"I was struggling with back pain for years before meeting Dr. Nimish, and I’m so glad I did. After a thorough consultation, he recommended a minimally invasive procedure, and I was back to my routine in no time. I can't thank him enough for giving me my life back!"
Abdurrahman
“ I am very grateful ”
"I’ve seen several doctors for my chronic neck pain, but none were as attentive as Dr. Nimish. He took the time to listen to my concerns and suggested a treatment plan that worked perfectly for me. I’m now pain-free and can do things I haven’t been able to for years.
Aaliyah Abbas
“ I'm Finally Painfree ”
"I came to him with a complex spine issue, and not only did he explain everything in a way that I could understand, but he also gave me options to consider. The surgery went smoothly, and my recovery has been much easier than I expected. I’m finally pain-free and feel like myself again!"

Your back deserves the best care
Get expert care today and feel the difference!











.png)